Cervical insufficiency
typora-copy-images-to: ....\Attachments
Cervical Insufficiency
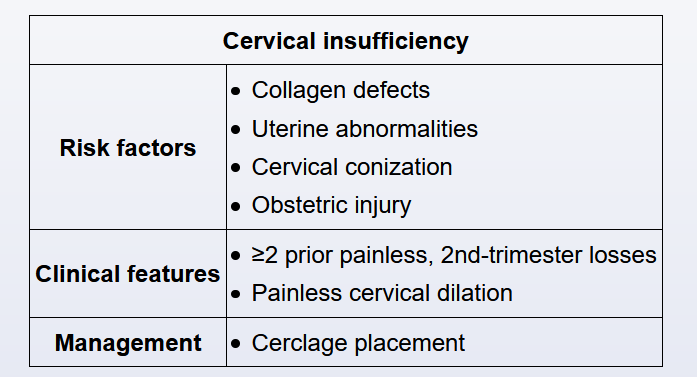
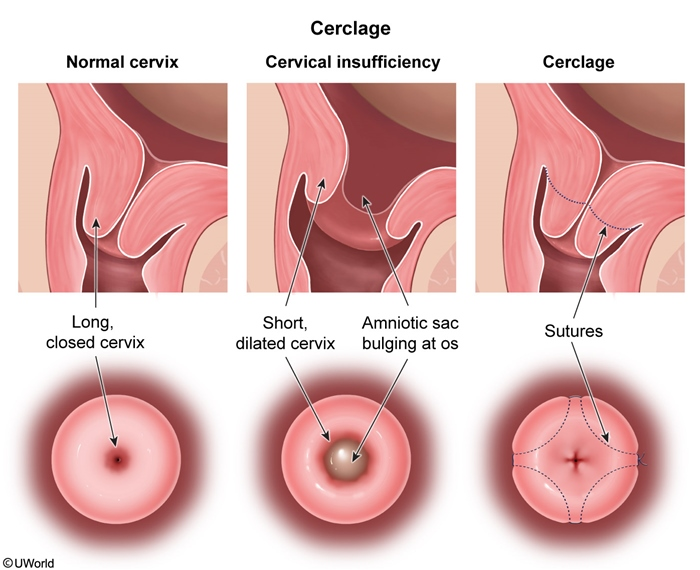
This patient has cervical insufficiency, a structural weakness of the cervix that predisposes to painless (ie, no uterine contractions) cervical dilation and second-trimester pregnancy loss. However, such patients can present with pelvic pressure when the gestation distends the vagina, with an increase in vaginal discharge due to loss of the mucus plug, or with light vaginal bleeding (eg, bloody show). Bulging or prolapsing amniotic membranes can also be present.
The diagnosis of cervical insufficiency can be based retrospectively on >2 prior painless spontaneous second-trimester losses. It can also be based on presentation of painless advanced cervical dilation at <24 weeks gestation in the current pregnancy. Risk factors include collagen abnormalities (eg, Ehlers-Danlos syndrome), uterine anomalies (eg, septate or bicornuate uterus), obstetric trauma, and surgical trauma (eg, cold knife cone).
Cerclage placement, a procedure during which a suture is placed to reinforce the cervix, has been generally shown to prevent second-trimester loss and preterm delivery in patients with cervical insufficiency. In patients with a history-based diagnosis, a prophylactic cerclage is placed at 12-14 weeks gestation. In patients with second-trimester, painless cervical dilation in the current pregnancy, cerclage placement is typically performed at diagnosis.
Prolapsing amniotic membranes, as seen in this patient, are a predictor for imminent (ie, within the next several days) delivery and indicate a poor prognosis. Prolapse of the membranes into the vagina causes prolonged exposure to vaginal flora and a high risk for intra-amniotic infection (chorioamnionitis), preterm membrane rupture, abruptio placentae, previable or preterm delivery, and maternal mortality. Prolapsed membranes are a relative contraindication to cerclage placement due to a high risk for iatrogenic membrane rupture. Therefore, even with cerclage placement, the prognosis for this pregnancy is poor, and the most likely outcome is a previable or preterm delivery